In the morning, I was with Tim at the heme/onc department, shadowing Dr. Chen. It seems like there were quite a few metastatic cancers, mostly to the lung. I was curious about this and ended up looking it up online afterwards. There are some theories about why there seems to be a preference for certain organs (a phenomenon called organotropism). One is that these are sites that are easier to reach by mechanical means by anatomical proximity or through blood (which doesn’t always explain some examples, such as the fact that lung cancers often metastasize to adrenal glands and ovarian cancers often go to the lungs). Another is that these sites are similar environments to the region where the cancer cells originated (for example, melanomas spread to the brain because they arise from the same embryonic cell lines, and breast cancer cells that use calcium in breast milk spread to bone to use the calcium there). It’s actually a pretty interesting topic that I might want to read up on later.
But I digress. We went through the patients all pretty quickly but these are the few scribbled notes on the patients we saw:
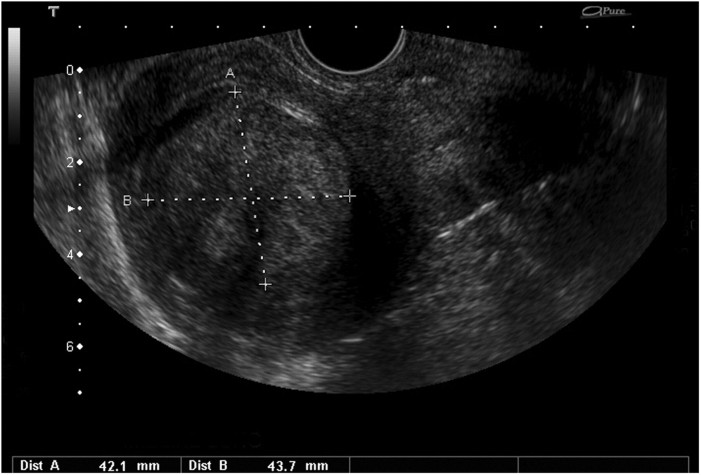
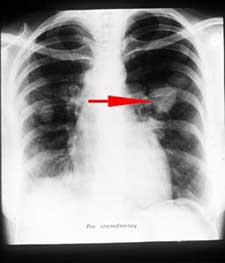
Patient 1: Neuroepithelial carcinoma (which we haven’t learned about yet and looks really complex because of the many different cell origins and grades) with lung metastasis treated with cisplatin, 5-FU, paclitaxel, and more recently methotrexate. Her WBC count was very low, 1500, so she was also treated with G-CSF and prophylactic antibiotics. As a side effect of the MTX, she also had mucositis. She also has a fever with unknown cause, but pneumonia is suspected based on the appearance of the CXR. However, some other physicians that Dr. Chen consulted with believe it’s actually just tumor fever (which apparently occurs in 7-31% patients with malignancies and is likely caused by cytokine release due to cancer-related mutations or necrosis).
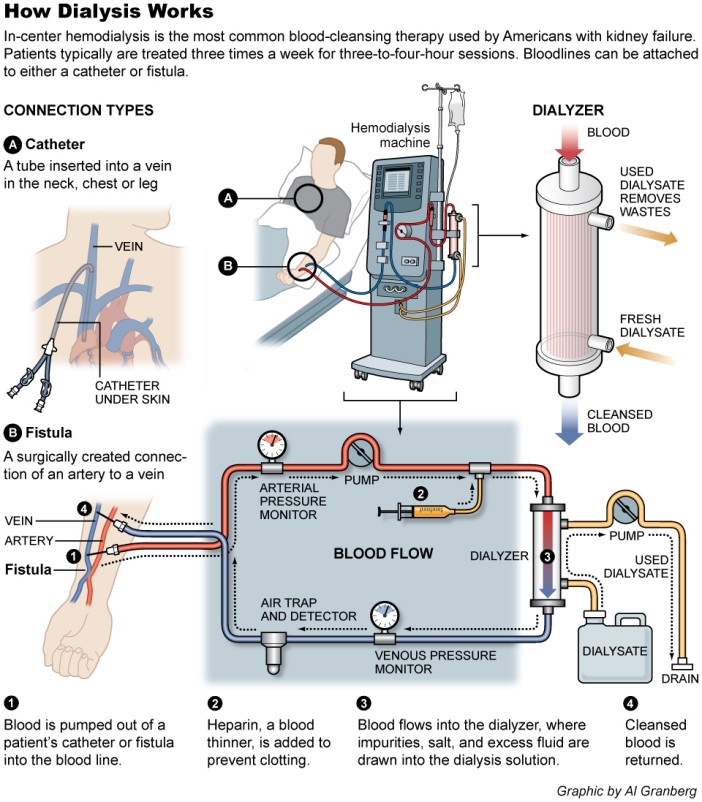
Patient 2: Diffuse large B cell lymphoma (DLBCL). She was treated with 6 cycles of rituximab (targets CD20) and went into complete remission, but now a new tumor was found in her oropharynx. She was treated with radiation, but ended up developing a candida infection that is likely catheter related. She seemed to also be taking glutamine and I wasn’t sure why until I later saw a poster saying that glutamine can polarize cancer from healthy cells. I couldn’t read the rest because it was in Chinese, but a quick search on pubmed reveals that glutamine supplements in cancer patients may be beneficial because many tumors are glutamine traps and end up leaving the patient glutamine-depleted.
For review, DLBCL is a lymphoid, non-Hodgkin lymphoma that is considered an aggressive cancer. It’s CD20+, CD30+, CD5+, and BCL6+, which explains why rituximab would work. The usual treatment we were taught for DLBCL is R-CHOP: rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone. Dr. Chen only mentioned rituximab, but it seemed to have worked really well until her new tumor was discovered. I’d imagine that this would be incredibly frustrating for Dr. Chen to see a patient come back after complete remission. It must also be frightening for the patient as well, knowing in the back of their mind that their cancer might come back at any time. This is probably a field I would not enjoy much. I don’t have the stamina to fight an uphill battle for so long.
Patient 3: Terminal pancreatic cancer with a prognosis on <6 months. He was treated with surgery and adjuvant therapy, but it recurred in the abdominal wall. He was then started on gemcitabine, but had no response, only suffering from decreased appetite, abdominal distention, nausea/vomiting, cachexia, and a candida infection. He was given parenteral nutrition but Dr. Chen mentioned that patients with his kind of cancer often die from malnutrition or infection.
Common metastasis sites of pancreatic cancer: liver, lung, peritoneum
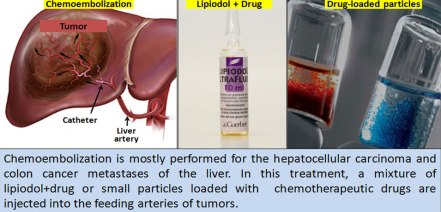
Patient 4: Metastatic (to the lung?) colon cancer with k-ras mutation (and presumably also a VEGF mutation because of the treatment choice even though Dr. Chen didn’t specifically mention it). Treated with a VEGF mab (bevacizumab) for 6 cycles. New symptoms of nausea.
Common metastasis sites of colon cancers: liver, lung, peritoneum
Patient 5: Atypical presentation in that she presented with exertional dyspnea, so they originally thought it was pulmonary TB. Also had constipation and bloody stools for weeks, so they found that it was sigmoid colon cancer with metastasis to lungs. It’s nearly obstructing the bowels so they suggested colostomy but she refused because she thinks it means it’s a poor prognosis. 2 cycles of chemo so far resulted in shrinkage. Dr. Chen later mentioned irinotecan as a colon cancer drug that can also cause diarrhea, so I’m not sure if that was the drug used for this patient or not.
Common metastasis sites of colon cancers: liver, lung, peritoneum
Patient 6: Hepatitis B virus related hepatocellular carcinoma. Usually treated with surgery, but this has already progressed too far. Treated with a drug that can prolong life for 2 months with increased GI bleeding risk, but it’s enlarging still. Dr. Chen mentioned that HBV and HCV related hepatocellular carcinoma is common in Taiwan because many people are carriers (10% for HBV, 15-20% for HCV).
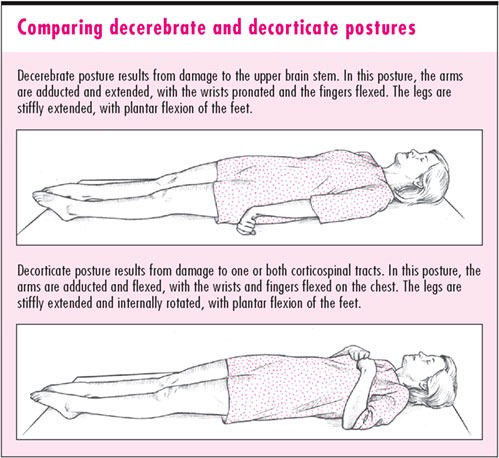
Patient 7: Lung adenocarcinoma with EGFR mutation. Treated with erlotinib but it progressed after 6-8 months. Suspected RLL pneumonia too so she’s being treated with a broad spectrum antibiotic. Dr. Chen noted shallow and low respiration, so he ordered an ABG to check for CO2 retention. Results showed a pCO2 >100 mmHg (normal is 35-45 mmHg).
Common metastasis sites of lung cancers: adrenal gland, bone, brain, liver, other lung
Patient 8: Cervical cancer recurrence with retroperitoneal metastasis. It was treated with surgery >10 years ago but came back last year. Enlarged lymph node on left side of neck. Also got sepsis and is being treated with antibiotics.
Patient 9: Lung adenocarcinoma with pericardial and pleural effusion. Patient complained of inflammation at site of IV catheter in arm.
Common metastasis sites of lung cancers: adrenal gland, bone, brain, liver, other lung
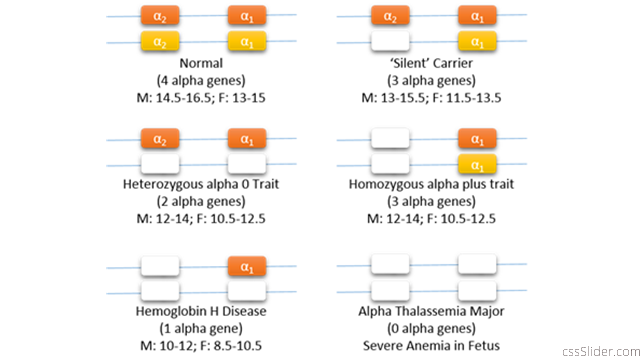
Patient 10: Severe iron deficiency microcytic anemia. Complains of hypogastric pain, found an ulcer, treated with proton pump inhibitor.
With this, I realized I needed to review chemotherapy drugs because I barely remembered much about them. Of the ones mentioned:
Cisplatin: a platinum analog and alkylating agent, major side effect to watch out for is nephrotoxicity. Dr. Chen mentioned that Taiwan’s insurance only pays for the less toxic 2nd generation version, carboplatin, when the patient starts showing signs of renal damage.
Methotrexate: S phase specific folate analog, inhibits DHFR, can result in mucositis
5-FU: pyrimidine antagonist that blocks thymidylate synthase
Gemcitabine: also a pyrimidine antagonist, Dr. Chen mentioned that this is standard for metastatic pancreatic cancer.
Paclitaxel: a taxane made from the bark of the Pacific yew tree, blocks microtubule disassembly, M phase specific, can result in peripheral neuropathy, usually used for breast, ovarian, and lung cancers
Irinotecan: a camptothecin made from the Mappia Foetida plant, inhibits topoisomerase I
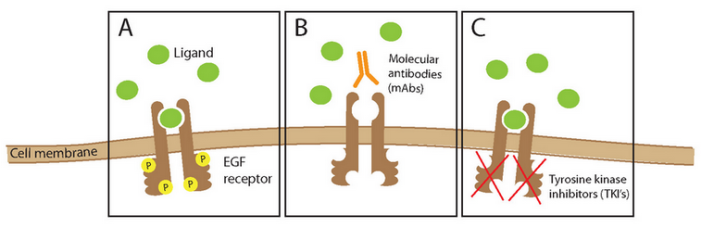
Cetuximab: EGFR targeting mAb, usually used for colon cancer
Bevacizumab: VEGF targeting mAb, inhibits angiogenesis
Rituximab: CD20 targeting mAb, treats non-Hodgkin’s B cell lymphomas, B cell leukemias
Erlotinib: EGFR targeting tyrosine kinase inhibitor, usually for non-small cell lung cancers
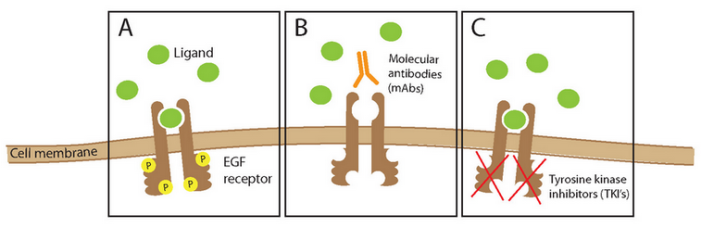
(A – ligands usually bind to the EGF receptor, leading to dimerization and phosphorylation of intracellular domains, eventually leads to K-ras activation and activation of growth factors, B – mAbs such as cetuximab bind to the receptor to prevent the ligand from binding, C – tyrosine kinase inhibitors such as erlotinib prevent phosphorylation)
Screening for mutations (usually amplifications) for EGFR and VEGF are therefore very important for determining which drugs to use. EGFR is especially important because aberrations occur more often in Asian populations (35% compared to the usual 10-25%). HER2 is also necessary in determining treatment for breast cancer, but we haven’t seen any cases of that yet, surprisingly enough.
Even though mabs are expensive, we learned that they are still paid for by the government, but only for a limited period of time. For example, cetuximab is approximately 180000 yuan/month and is only covered for 6 cycles. Dr. Chen estimates that less than half of patients need it for more than this amount of time, however.
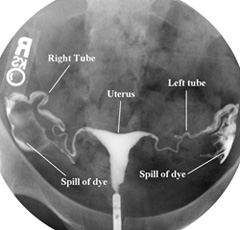
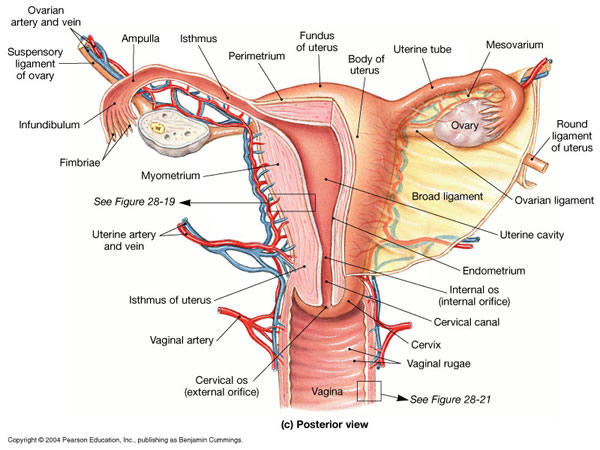
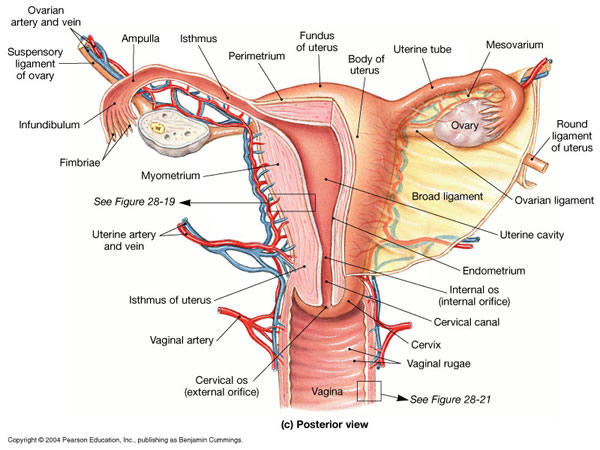
Later in the afternoon, I got to watch a myoma removal through total hysterectomy. It was large, maybe about the size of a papaya, so Dr. Cao, the ob/gyn, said that it could not be removed laparoscopically. He made a midline cut on her abdomen and dissected until he reached the uterus. First, he cut the round ligament because it contains no blood vessels, then the suspensory ligament of the ovary (which Dr. Cao called by another name, the IPL / infundibulopelvic ligament) which contains the ovarian artery and vein. Because the patient was pre-menopausal, he opted to leave the ovaries, so that she could still produce the proper hormones. Next, Dr. Cao cut the uterine artery and vein, and took the uterus out along with the cervix.

This was amazing to watch. I had never seen such a huge tumor and I can’t believe the patient had been carrying that thing around in her body. I was fascinated; I realized that I would probably enjoy ob/gyn a lot more than I would have expected. What I like is how they get to interact quite a bit with their patients but also perform surgeries, which sounds like a good mix of surgery and medicine. I may actually end up liking this specialty (up until I witness a particularly messy and painful childbirth perhaps).