Today we rounded on the same patients again. Since cancer is more of a chronic progressive disease and the chemo treatments take a few cycles to show any signs of working, nothing really changed since we last saw them.
However, today, the patient with hepatocellular carcinoma had a family member visit, so Dr. Chen had to give her the bad news about his prognosis. He was clear and concise in telling her that the patient has been unconscious / comatose and is unlikely to improve. She started sobbing and it was heartbreaking to see. Dr. Chen said that it’s always hard to do even now, despite the fact that he’s been doing this for years. That’s is both a comforting and uncomfortable thought. On one hand, it’s good that even after all this time, Dr. Chen is an example of a physician hasn’t lost his sense of empathy for patients and their families despite being in a specialty that requires him to give bad news quite often. On the other hand, that also means that it will never get any easier. I don’t know how he deals with it. I don’t think I could.
In ob/gyn, I was in the outpatient clinic this time. A majority of it was pap smears, but I also got to see some interesting things, such as a myoma on ultrasound, a cervical polyp, a hysterosalpingogram (HSG), and a 28 week old fetus on ultrasound.
I learned that myomas are usually benign and are only considered for removal according to these criteria:
- If the myoma is >5 cm (but this is not absolute. If it’s not causing any other problems, it doesn’t need to be removed either)
- If the myoma is symptomatic (which include pain, constipation, abnormal bleeding)
- If the myoma is growing rapidly
Myomas are often hormonally-related and will often shrink when the patient hits menopause, so if the patient is around 45-50 years old, instead of choosing surgery, they can also just treat the symptoms until then.
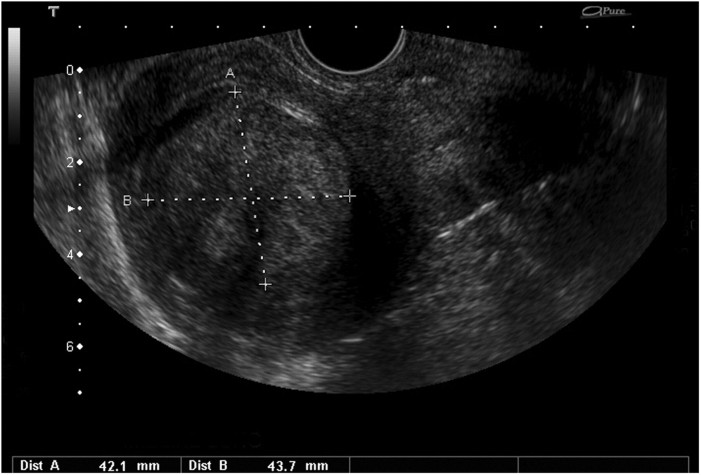
(The patient had a rather large myoma but it wasn’t causing symptoms yet so Dr. Cao didn’t think it should be removed)
The HSG was test used to determine if there is an anatomical reason for infertility. Dye is injected into the uterus and fallopian tubes to check for blockages. The procedure looked incredibly painful though because not only was the speculum rather large, she also had these tenaculums clamped onto her cervix to keep it open:

(Like pointy medieval torture devices)
I felt bad for her. It seems like most gynecological procedures are rather uncomfortable for the patient. Even pap smears produce some discomfort for a lot of patients, often due to the speculum. Isn’t there a better way of doing this?
Still, the HSG itself produced some pretty cool images. And the patient got some good news out of it: she had no obstructions in her fallopian tubes and everything was anatomically normal.
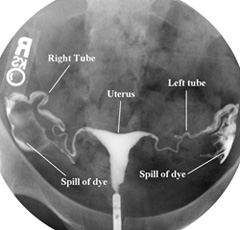
(It’s not typically this clean of an image though. The timing is hard to get right)
After even more pap smears, we ended the day with a check up on a 28 week old fetus.

Dr. Cao measured the biparietal diameter (BPD) and abdominal circumference (AC) of the fetus in order to estimate the weight. He then checked to see if everything else was developing normally, such as the heart, face, spine, etc. The parents were a little worried about the baby’s weight, so they were glad to hear that everything was completely normal. What a great way to end the day.